The Indian Keratoconus Foundation
The Indian Keratoconus Foundation (IKCF) is a dedicated outreach platform to increase awareness and understanding of Keratoconus.
In India alone, it is estimated that 2.3 % population is affected by Keratoconus.
We aim to provide appropriate guidance and access to resources that may help you to understand and deal with Keratoconus better. Through the IKCF, we hope to enable empowerment of patients and their parents by connecting people dealing with Keratoconus to experts and relate to others living with Keratoconus for their emotional well-being.
It is estimated that 2.3 % of our population in India may be affected by Keratoconus. As this condition strikes early, but is usually diagnosed at a later stage, we believe it is of paramount significance to spread awareness and provide access to relevant resources about Keratoconus.
Mission and Vision
Enable uniform and easy access to information about Keratoconus and to allow patients to connect with each other and share their experience in dealing with this disease.
What is Keratoconus
The cornea is a clear, dome-shaped tissue at the front of our eyes that helps eyes to focus light enabling clear vision. Keratoconus is an eye condition in which the normally round, dome-shaped cornea progressively thins, and gradually bulges outwards like a cone. The change in shape of cornea causes blurry and distorted vision, thereby making daily tasks such as reading or driving difficult.
Symptoms of Keratoconus
- Round objects appear to be oval
- Frequent change in spectacle power
- Blurred & distorted vision; straight lines look bent or wavy
- increased sensitivity to light and glare
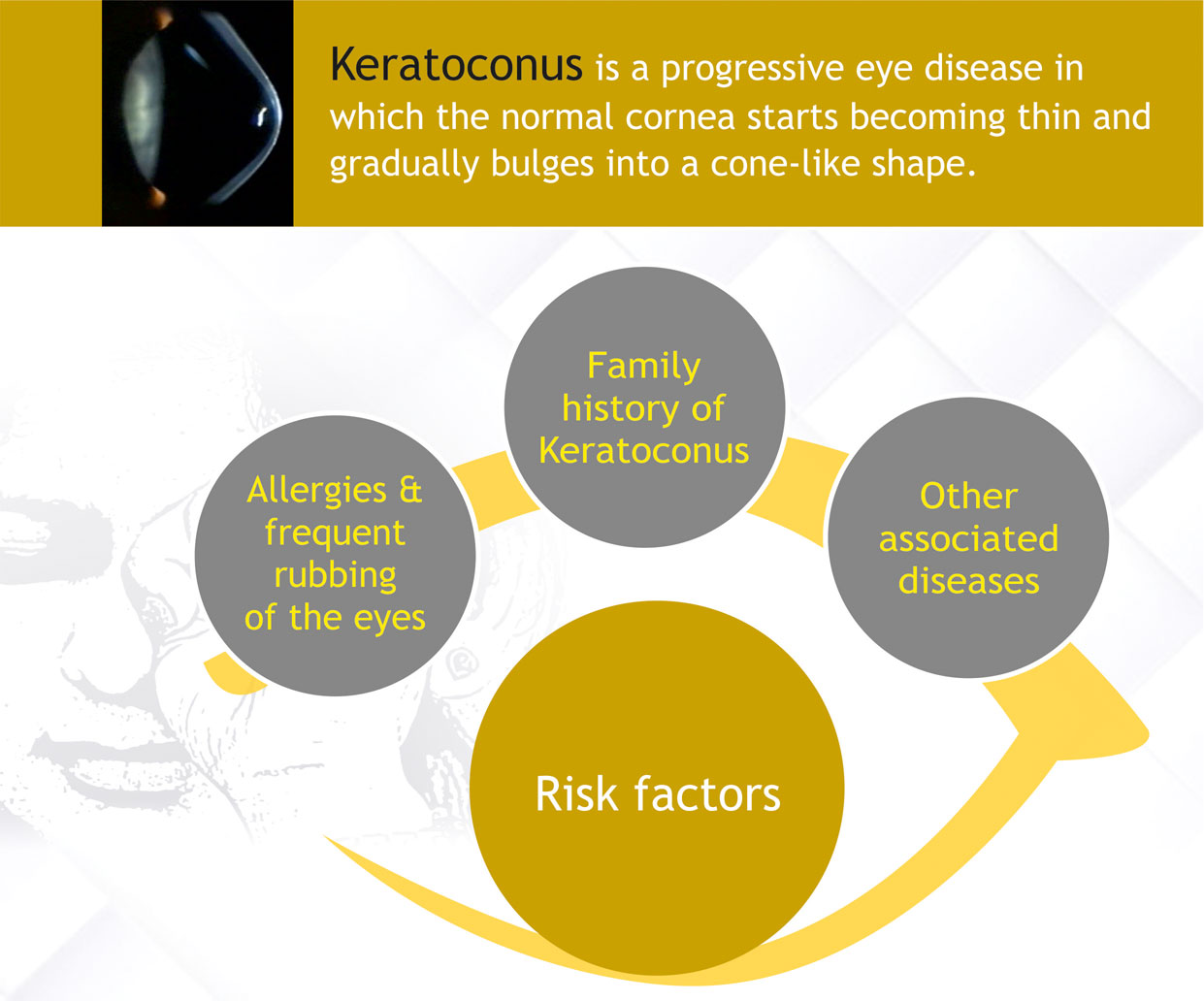
What Causes Keratoconus
The exact cause of Keratoconus is unknown. There are many theories based on research and its association with other conditions. However, no one theory explains it all and it may be caused by a combination of things.
It is believed that genetics, the environment and the endocrine system, all play a role in Keratoconus.
Many who have keratoconus report vigorous eye rubbing and also have allergies (which cause eye itching and irritation, leading to eye rubbing), however the link to allergic disease also remains unclear. A higher percent of keratoconic patients have atopic disease than the general population. Disorders such as hay fever, eczema, asthma, and food allergies are all considered atopic diseases. Those with KC are advised to avoid eye rubbing as much as possible.
It is important to understand the nature of keratoconus, and to develop a positive attitude of learning to live with this lifelong condition. Keratoconus is manageable.
Living with Keratoconus
People react differently to the news that they have Keratoconus (KC). Lack of knowledge often creates fear, so learn all that you can about this condition. Ask questions and discuss your concerns with your doctor and others who have Keratoconus. This will be both enlightening and reassuring. While it is important that you accept Keratoconus as a fact in your life and realize that you have to adapt to it, it is essential for you to understand that adapting is not surrendering. You control your life, keratoconus does not!
From a medical standpoint, the most important thing you can do is to keep in touch with your eye care practitioner and follow his/her instructions.
From an emotional and psychological standpoint, it is important to understand the nature of Keratoconus and to talk freely about it with family and friends to be sure that they understand it.
Perhaps there is no better therapy than sharing your experiences with others in similar circumstances. If at all possible, talk with other keratoconus patients. The mutual sharing of common experiences is both rewarding and reassuring. For information about support group in your area, contact us.
Hear from some Kerataconic patients
Master Shukri Murhad Sarhan, 11, from Yemen treated for advanced keratoconous
PROSE Lenses Have Been a Boon for Sandeep
Mirchi Shadab on early detection and care for Keratoconus
Shanmukha’s Remarkable Recovery After Eye Disorder
Treatment Options
There are a variety of treatment options for keratoconus that divide into two categories. The first objective is to stop the disease from getting worse. This is done by treating associated conditions such as allergies to prevent rubbing of the eyes. Collagen cross linking is a treatment that has shown very promising results in stopping progression of keratoconus.
Surgical Treatment Options
Intra Corneal Rings are plastic rings inserted into the cornea that flatten the cone.
Corneal transplantation: the abnormal corneal shape is removed partially or entirety and is replaced with a healthy donor cornea tissue. Corneal transplants are the last resort as there is significant recovery time and follow-up care required.
Reach Us
Administrative Office
L V Prasad Marg, Banjara Hills, Hyderabad
18002002211





